Four lost pregnancies. Five weeks of IVF injections. One storm.
Published 2:00 pm Wednesday, July 3, 2024
Four lost pregnancies. Five weeks of IVF injections. One storm.
On their very first date, Kirsti and Justin Mahon talked about wanting kids. They met on a dating app in 2016, nine months after Kirsti moved from Texas to Florida. Almost immediately, they fell in love.
A little over two years later, they got married. Six months after that, they started trying for a baby. To their surprise, they got pregnant right away. But just as quickly, they had an early miscarriage. At 27, Kirsti didn’t have any reason to suspect fertility problems, and her obstetrician was quick to reassure her: Kirsti’s blood work looked normal, and getting pregnant after a month of trying is a good sign of fertility. Conceiving again, she was told, would be easy.
As she told The 19th, over the next two years, Kirsti got pregnant three more times. None of her pregnancies lasted beyond the first trimester.
“It felt like we were hitting a brick wall,” Kirsti said. In January 2022, the couple went to see a fertility specialist who conducted a series of intensive tests that uncovered what was really going on. Kirsti was only 29 years old at the time, but the specialist told her that her egg quality was that of a 40-year-old’s. In vitro fertilization, or IVF, the specialist said, was Kirsti and Justin’s best hope.
It didn’t take the couple long to decide to take the plunge. “With every loss that we had it was like I was watching Kirsti lose a piece of herself,” said Justin. “It became obvious with the consultation that the IVF process was really the only way to guarantee that this really brutal cycle wouldn’t continue.”
So they drained their savings, cashed in an old retirement account, and took out two loans to pay for the treatment. They live in Florida, a state where coverage isn’t mandated, so most of the procedures would be out of pocket. Justin estimates it cost between $25,000 and $30,000. The couple hammered out the minutiae of IVF with their specialist, down to the timing of every hormone shot. They felt ready.
But Kirsti and Justin hadn’t accounted for hurricane season.
If the process of getting pregnant naturally feels murky and unpredictable, in vitro fertilization turns conception into a science — every menstrual phase, reproductive hormone and embryo carefully screened, tested, and optimized. First, patients inject themselves with fertility hormones aimed at stimulating ovarian follicles and bringing as many eggs as possible to maturity. An IVF cycle can fail right then and there, with the bad news showing up on an ultrasound screen or on the printed pages of a laboratory test before the eggs are even collected. Often, too few follicles develop. Ovulation can happen prematurely, or the ovaries can become hyperstimulated, causing pain, nausea, or more serious health problems. Everything can go wrong, and everything — down to the timing of each hormone shot — needs to go right.
If it does, the patient’s eggs are removed for fertilization in an outpatient procedure called an egg retrieval. The eggs must be harvested 34 to 36 hours after the “trigger shot,” a final hormone injection which prompts the eggs to finish maturing, but before the ovary releases them into the fallopian tubes. Patients are administered a painkiller, then the doctor guides a needle through the vagina or stomach and into the ovaries, aiming to suction all the eggs from their follicles. Mature eggs — there can be dozens, just one, or none at all — are fertilized with sperm in vitro, Latin for “in the glass,” or in this case in a petri dish. There, the embryos mature for three to six days. Not all of them survive, or develop correctly. The ones that make it can be reinserted into the uterus right away or, more commonly, frozen for later use.
Two time-sensitive procedures bookend the most stressful and critical weeks of the IVF process. The first is the egg retrieval. Once the trigger shot has been administered, there’s no turning back. If the procedure doesn’t take place approximately 36 hours after the injection, the patient’s follicles rupture, casting the precious eggs irretrievably into the fallopian tubes. A missed alarm, a traffic jam, or a delayed flight can wreck an enormous financial and emotional investment.
The second is the embryo transfer. A patient’s uterine lining must be sufficiently thick when an embryo is reinserted — otherwise, the embryo won’t implant, and the patient won’t get pregnant. Doctors often prescribe additional hormone injections for up to 12 weeks to boost estrogen levels and thicken the uterine lining before a frozen embryo is thawed and transferred. Fertility clinics typically require patients to come in regularly for ultrasounds to determine the optimal day for the transfer. If the lining remains too thin, or if the patient’s menstrual cycle advances too far, then the transfer must be delayed for at least another month.
These windows of opportunity are narrow, and it doesn’t take much to slam them shut. For a growing number of would-be parents living in the coastal areas of the United States, where climate change is making hurricanes faster-moving and more intense, all it takes is a single storm.
In September 2022, the Mahons were preparing for the final stage of IVF: the embryo transfer.
Kirsti had already undergone the grueling egg stimulation and retrieval process, which produced 23 eggs. Four had turned into embryos, and three were genetically tested. Two came back healthy and had been frozen.
Her transfer had initially been scheduled for August, but it got canceled when Kirsti contracted COVID-19 that July. Now, as summer turned to fall, Kirsti spent five weeks injecting herself with hormones at their home on the outskirts of Naples, Florida, where she worked as an animal supervisor at the area zoo. Naples sits on Florida’s Gulf Coast, about 40 miles north of the northern edge of the Everglades.
Less than a week out from her transfer, she was at the clinic for a final ultrasound and some blood work when she asked whether she should be worried about a coming storm she had seen on a weather forecast. She remembers the nurse telling her, “We’ll keep an eye on it, but I really wouldn’t worry about it.” At that time, the storm system still looked like it might miss Naples.
By the weekend, though, what had started out as a tropical depression whipped itself into Hurricane Ian, which would turn out to be one of the deadliest and most destructive in U.S. history.
That Monday, Kirsti and her husband had grown increasingly worried, so they emailed the fertility clinic for an update. While they waited to hear back, they tracked Hurricane Ian on the news, watching as it made its way toward the U.S. “It just kept getting scarier and scarier,” Kirsti said.
On Tuesday, Kirsti went into work and started to evacuate animals from their outdoor enclosures. At this point, the hurricane began to veer toward southwest Florida, but was still expected to make landfall more than a 100 miles north of Naples, sparing her town. That afternoon, calls began to stream in from her parents and her in-laws, who lived along the Florida coast. It was decided that they should take shelter in the couple’s house. By that evening, Kirsti’s two-bedroom, one-bath house was suddenly packed with family and a menagerie of pets.
On Wednesday morning, Justin injected Kirsti with the last dose of her medication. Southwest Florida was flooding, and parts of the state were losing power, but they hadn’t heard anything from the clinic. Their appointment was supposed to be the next day. As far as Kirsti knew, the procedure was still on track.
Since the beginning of the 2000s, climate change researchers have warned that a warmer planet produces stronger and more damaging hurricanes. In 2020, 30 named storms developed in the Atlantic, setting a record. University of Pennsylvania researchers recently predicted that this year’s Atlantic hurricane season will include 33 named storms. Study after study has demonstrated that the convergence of a warmer, wetter atmosphere and a higher sea-surface temperature causes tropical depressions to grow into hurricanes more quickly. A study published late last year said storms have become twice as likely to develop from a weak tropical cyclone into a Category 3, 4, or 5 hurricane within a 24-hour window — a process meteorologists call “rapid intensification.” The growing intensity of hurricanes has prompted some climate scientists to suggest adding a sixth category to the Saffir-Simpson scale, for hurricanes with winds faster than 192 miles per hour.
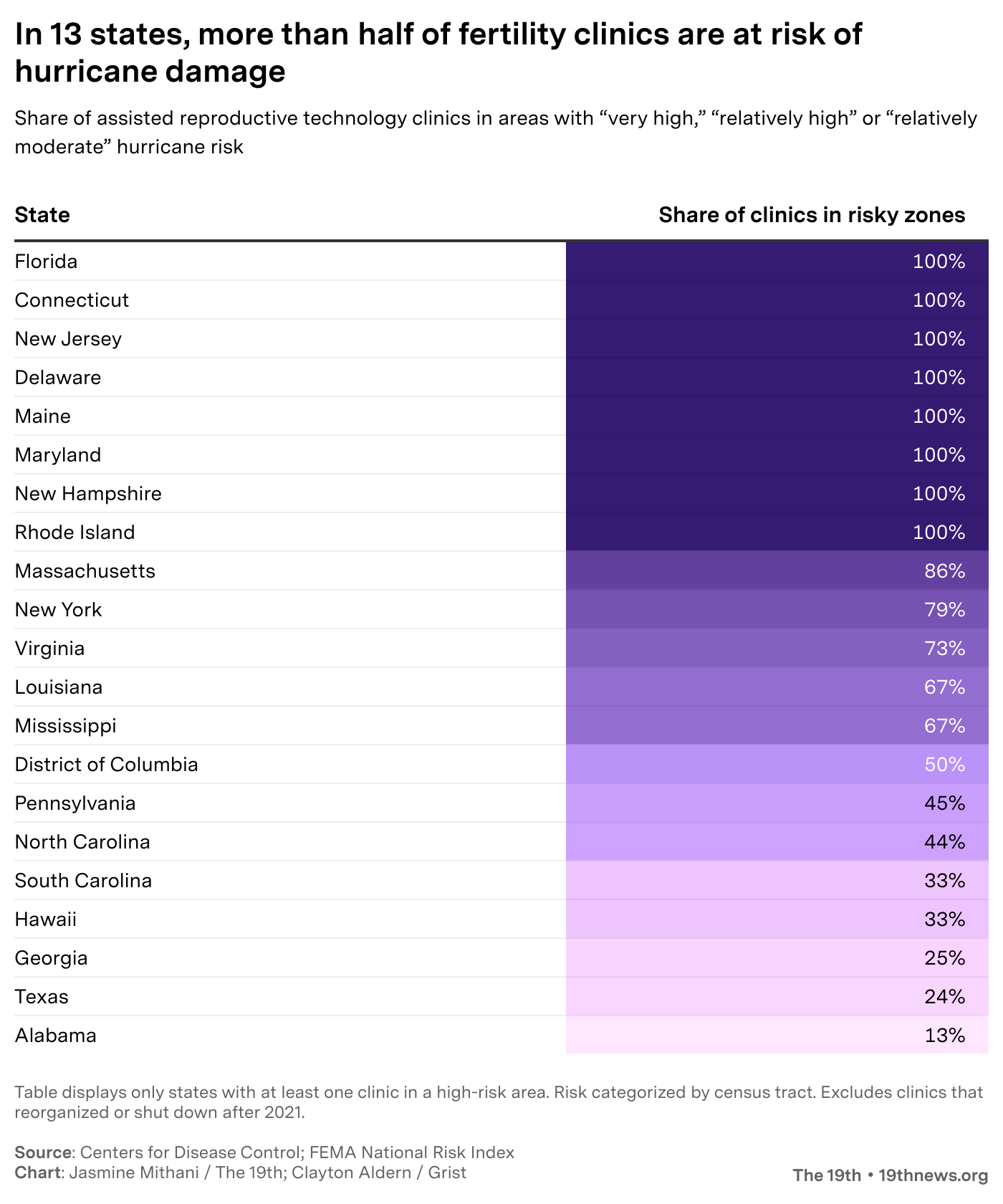
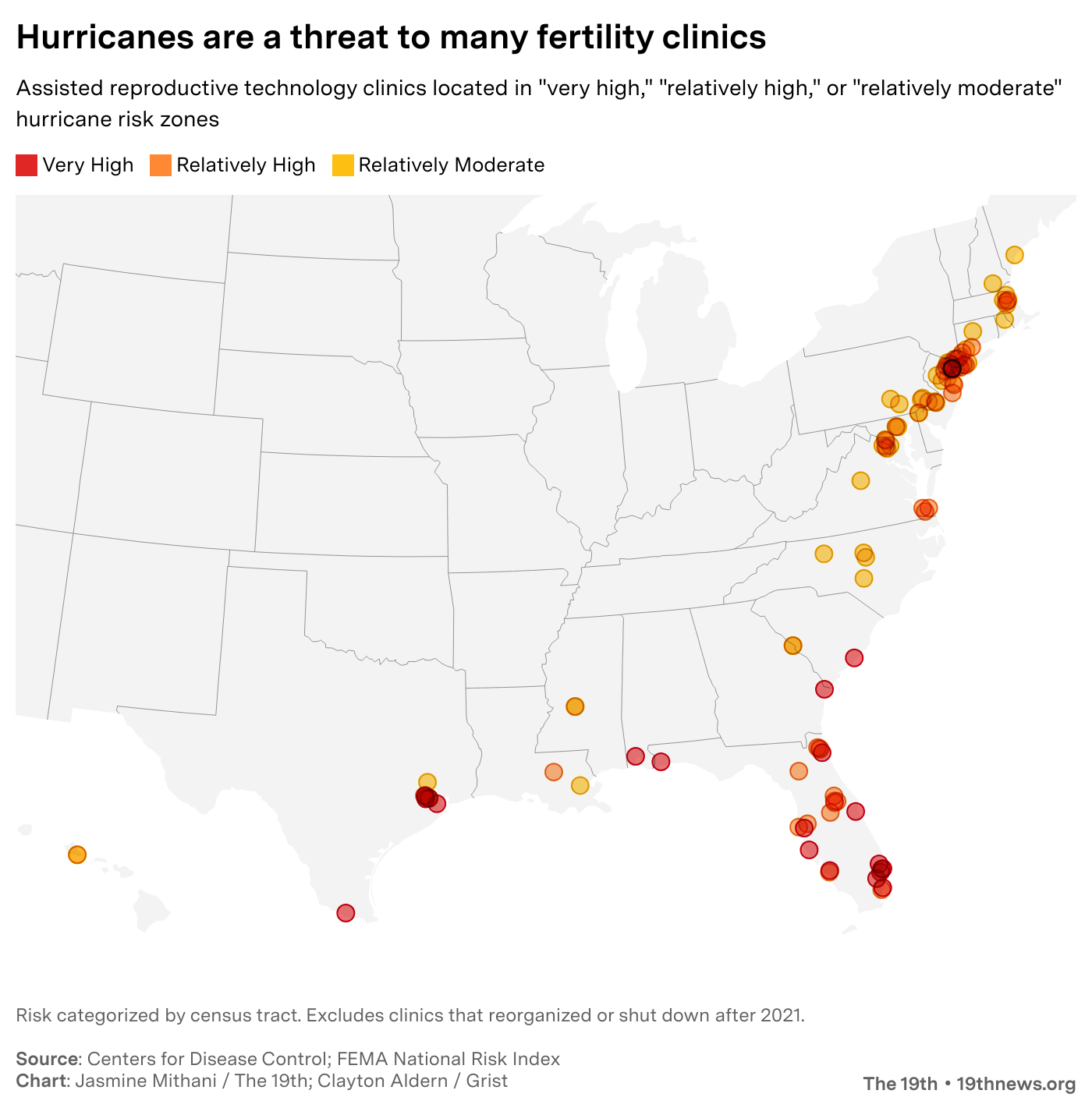
Hurricane Ian was a prime example of a storm charged by climate change. It strengthened from a Category 3 into a Category 4 hurricane in under 24 hours. Ian is just one of several major hurricanes that have struck the southern and southeastern coasts of the United States in the past decade — regions that are particularly vulnerable to damage during the Atlantic hurricane season. In places like Florida, Louisiana, Georgia, Puerto Rico, and Texas, it’s becoming increasingly evident that communities and the infrastructure they rely on are ill-prepared for intensifying storms.
![]()
Jasmine Mithani // The 19th; Clayton Aldern // Grist
Fertility clinics not immune to the havoc caused by hurricanes
Hurricane Harvey, a Category 4 storm that hit Texas in 2017, submerged hundreds of roads, collapsed bridges, and damaged more than 300,000 homes. That same year, Category 4 Hurricane Maria decimated Puerto Rico’s aging power grid, plunging the island into darkness for nearly a year — the longest power outage in U.S. history. In 2020, Category 4 Hurricane Laura barreled into southwest Louisiana, displacing thousands of residents and nearly destroying the city of Lake Charles. The city was still clearing wreckage caused by Laura, the most powerful storm to hit southwest Louisiana since record-keeping began, when another hurricane, Category 2 Delta, carved a nearly identical path of destruction through the state. Lake Charles continues to recover four years later.
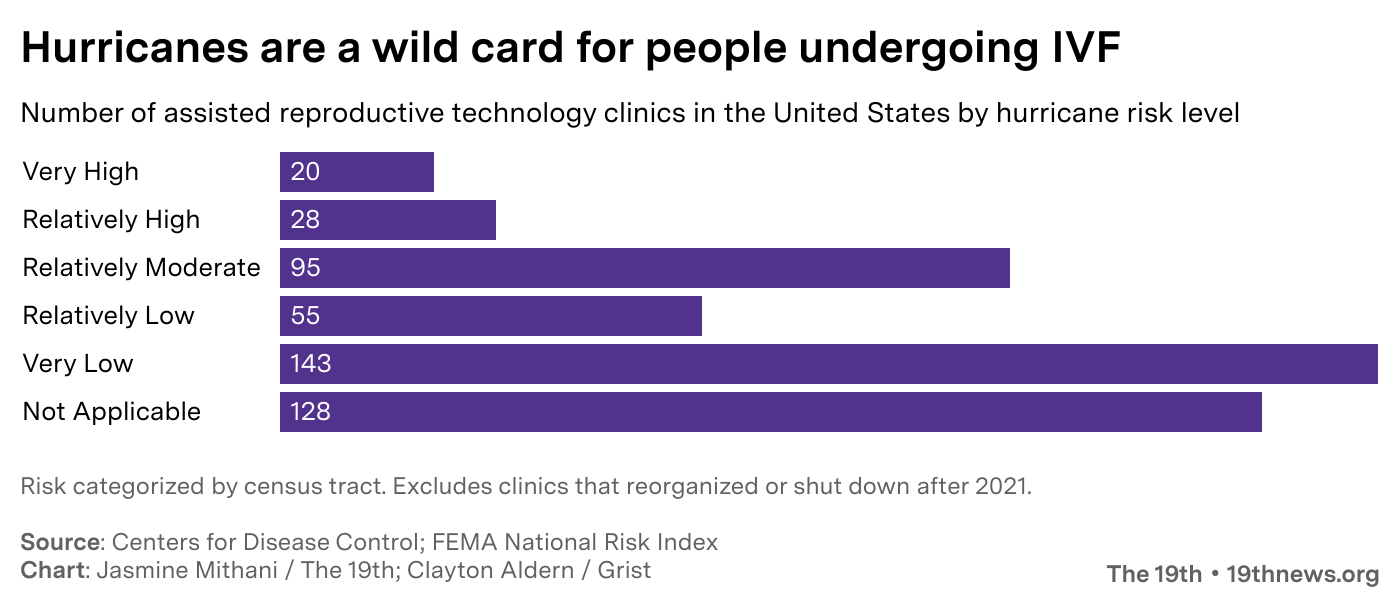
Fertility clinics are just as vulnerable to storms as any other infrastructure. When Hurricane Ida hit New Orleans in 2021, Nicole Ulrich, a doctor at Audubon Fertility Center, experienced firsthand the challenges intensifying hurricanes pose to these centers. Similar to Hurricane Ian, Ida progressed so rapidly that it caught the city and clinic off guard.
Forecasters “thought it was maybe going to be a [Category] 1 or a 2, and then it was going to be a 3, and then all of a sudden, it was going to be a 4. At that point, there really should have been a mandatory evacuation, but there wasn’t enough time,” said Ulrich. “We had to close the clinic at that point, because there just wasn’t another option.”
As a result, Audubon had to cancel at least 10 IVF cycles, and delay the start of several others. This included patients who were preparing for embryo transfers, and others who had started injecting the hormones needed for egg retrieval. The clinic also had some embryos growing in the lab. It usually takes five or six days to tell which embryos are healthy and suitable for freezing, but Ulrich’s clinic had to quickly decide to freeze them early, on days two and three instead, just in case their backup power generator failed.
Once the clinic was back up and running, it took months before Ulrich and her team could fit in all the patients whose cycles had been canceled or delayed — patients who were anxiously awaiting the chance to restart the process.
“For most people, waiting a month is not going to make that big of a difference. But when you’re in that moment and you’re 42 and you know your egg count is low, it feels like just the most devastating thing that could happen,” said Ulrich. “There is a chance that, especially when you get closer to 43, it might make a difference.”
The embryos Audubon froze early had to be thawed in order to mature and then refrozen. The clinic is still analyzing data from that change in protocol to understand if it affected pregnancy outcomes.
Jasmine Mithani // The 19th; Clayton Aldern // Grist
Clinics in Riskier Areas Encouraged to Consider Emergency Plans
Thanks to that experience, Ulrich published a paper in 2022 that calls for more research on the topic of IVF and climate change, with a focus on the particular challenges posed by rapidly intensifying hurricanes. “It had a huge impact on our clinic and our patients, and for months afterwards, we were still dealing with the aftereffects,” she wrote.
But the experience taught Ulrich lessons other IVF facilities could benefit from. Ulrich said she’d love to see clinics establish better relationships with other fertility treatment centers in their region so that patients could transfer to them in times of disaster. She also encourages clinic staff to review their emergency action plans to ensure they are prepared to meet the changing nature of storms, and to be ready to make decisions quickly to salvage cycles and protect embryos. All clinics store embryos in nitrogen tanks, which do not rely on electricity and are typically safe from blackouts or issues with electrical grids. But the labs that embryos mature in before they are frozen do depend on electricity — and if a disaster takes out power for too long, even backup generators can run out of fuel. During Hurricane Katrina, embryos were lost at one clinic for this reason.
IVF clinics are currently not required to have emergency plans in place, but it is recommended by the American Society of Reproductive Medicine. In 2022, the society published its own paper highlighting the need for clinics to adapt to increasingly threatening hurricane seasons.
“Clearly, climate change means you are having more extreme weather events, and [I] think that, like every other part of society, from homeowners to hospitals, fertility clinics have to think a bit more about how they can build more resilient systems,” said Scott Tipton, chief advocacy and policy officer with the American Society of Reproductive Medicine.
Within a few hours of Kirsti’s final hormone injection, she saw her nurse’s name light up on her phone. Before ducking into her bedroom to get some privacy from the houseguests, she exchanged a despairing glance with Justin. “I just looked at my husband and I was like, ‘It’s not happening, it’s not happening,’ and I took the phone call.”
The nurse immediately assured her that her embryos were safe but confirmed her suspicion: The clinic was closing because of the storm, and Kirsti wouldn’t be able to go through with the transfer the following day. In fact, they would have to start her cycle all over again. (Kirsti’s clinic did not respond to requests for comment.)
“It just felt like our earth was shattered,” she said. Five weeks of hormone injections had taken their toll on her body, both emotionally and physically. She had grown to dread the shots, which caused swelling in her buttocks, thighs, and stomach. “We had spent so much money, so much time. I was covered in bruises,” she said. “I hung up the phone and I just lost it. I lost it. I wasn’t even angry. I was just heartbroken.”
Jasmine Mithani // The 19th; Clayton Aldern // Grist
The Costs of IVF Loss Are Real
Aside from the sadness she felt over yet another hurdle in their fertility journey, Kirsti thought about all the money she and Justin had poured into the treatment, including borrowing from family. The $2,500 the couple had spent on fertility medications that month evaporated the moment Kirsti’s phone rang. If the couple were to restart the embryo transfer process, they would have to spend thousands more.
The average cost of one cycle of IVF in the U.S. is $12,400, but prices can vary depending on the clinic, the cocktail of fertility medicines used, and the number of embryos collected and frozen. Some clinics charge as much as $30,000 per cycle. And many patients need more than one cycle to get pregnant.
Because IVF is so costly, there is a large access gap between those who can afford the treatment and those who can’t. In a 2021 survey administered by researchers in Illinois who sought to better understand the demographics of IVF patients in the state, 75.5 percent of the respondents were white, 10.2 percent Asian, 7.3 percent Black, and 5.7 percent Latina.
Despite these hurdles, IVF is becoming increasingly popular. The treatment allows people to delay pregnancy for any number of reasons — to build a career, save money for a family, or find the right partner. And it’s a crucial tool for people struggling with infertility. In the U.S., that’s 1 in 5 women.
More than 40 percent of all American adults now say they have used fertility treatments or know someone who has had them, as the number of people who delay childbearing grows. In 1970, the average age of a person giving birth for the first time was 21.4. In 2021, that average was six years higher.
As IVF has grown more common, it has also become the target of political and legal attacks. In February, Alabama’s Supreme Court, dominated by conservative judges, ruled that embryos created in vitro should be thought of as children for the purposes of wrongful death lawsuits. The ruling had an immediate chilling effect on clinics throughout the state. A month later, Alabama lawmakers extended criminal and civil immunity protections to IVF clinics for their day-to-day operations. Manufacturers of products used in the course of IVF treatment get some immunity protections under the new law, too. But the law still leaves providers at risk because it doesn’t challenge the court’s assertion that embryos are people.
This decision also has possible implications for doctors practicing IVF when a disaster hits, said Ulrich. “If you had an incubator on a power grid that failed, and you didn’t have a backup or the backup failed — those embryos would have been lost,” said Ulrich. Perhaps patients would see the loss as an unavoidable accident — or perhaps they’d sue for wrongful death, she said. “It’s another reason to be careful.”
In the days after Hurricane Ian made landfall, Kirsti spent her time worrying about her family, her neighborhood, her house, and the animals at the zoo. Beneath it all, she felt a deep sense of despair. “I felt like every single piece of me was being hit and like every single thing I had was being ripped to shreds,” she said. But there was no doubt in her mind that she and Justin would try again.
For months, Kirsti’s embryos stayed safely frozen while she and a few other women she knew from the clinic waited to have their transfers rescheduled. The hurricane’s disruption meant their appointments would come after others already on the books, so she wouldn’t be penciled in until December, delaying her procedure even longer. The clinic agreed to waive the fees for the postponed transfer, but Kirsti and Justin still had to pay out of pocket for the costly medications.
On Halloween, she once again started preparing her body to carry a baby, taking a slew of medications and undergoing daily hormone injections. On the first of December, she completed the long-awaited transfer. Two weeks later, her doctors confirmed what she already knew based on a home test: Kirsti was pregnant. “I was over the moon,” she said.
She was also nervous: “We had been pregnant before and it always ended in loss.” As she and her husband put together the baby’s zoo-themed room they felt hopeful — but nothing was certain until Aug. 8, 2023, when she gave birth to a healthy baby girl named Gracie.
That day, the Naples coast was hot and sunny. As they looked down at their newborn daughter, Kirsti and Justin reflected on all it took to get there, after nearly four years of trying to start their family. “She was here and in our arms, and we just had this moment,” she said. “It was like, ‘We did it.'”
A few weeks later, Florida was hit by another Category 4 hurricane.
This story is part of the series Expecting worse: Giving birth on a planet in crisis, a collaboration between Grist, Vox, and The 19th that investigates how climate change impacts reproductive health — from menstruation to conception to birth.
Jasmine Mithani and Clayton Aldern contributed to this reporting.
This story was produced by The 19th and reviewed and distributed by Stacker Media.





