Healthcare deserts in 2025: 80% of the country lacks healthcare access
Published 7:00 pm Tuesday, July 29, 2025
Healthcare deserts in 2025: 80% of the country lacks healthcare access
More than 80% of U.S. counties — home to over 120 million Americans — still lack proper access to healthcare services, according to new data from GoodRx Research.
In 2021, GoodRx, a platform for medication savings, published its first comprehensive report on the state of “healthcare deserts” in the U.S. It identified areas that lack adequate infrastructure to ensure a healthy community, including access to pharmacies, primary care, hospitals, emergency services, and low-cost community health centers.
In 2025, access to critical healthcare services is still out of reach for millions of Americans. Since 2021, more than 1,300 pharmacies have closed, increasing the number of people living in pharmacy deserts. Supply of primary care professionals continues to lag behind demand, amidst federal funding withdrawals for shortage areas. And with the shifting policy landscape, hospitals and federally funded health centers remain at risk of closure.
Trending
Here’s how healthcare infrastructure 一 or lack thereof 一 continues to shape access to healthcare.
Key takeaways:
- Healthcare deserts are areas that lack adequate access to and infrastructure for healthcare services. They exist in about 80% of U.S. counties.
- New data from GoodRx Research shows that healthcare deserts continue to affect millions of people — roughly 1 in 3 Americans.
- Since 2021, pharmacy deserts have expanded across the U.S., and access to critical hospital services, including trauma care and hospital beds, has remained stagnant.
- Nearly 60% of counties have more than one type of healthcare desert. Healthcare deserts are also more likely to affect people with lower incomes and those without health insurance, further widening health disparities.
Pharmacy deserts spread, while hospital and trauma center deserts persist
Today, roughly 81% of counties across the U.S. are healthcare deserts of some kind, meaning the majority of the population lacks proper access to pharmacies, primary care, hospitals, hospital beds, trauma centers, or community health centers. GoodRx estimates show that over 120 million people currently live in a healthcare-desert county, accounting for roughly a third of the U.S. population.
GoodRx
GoodRx
GoodRx
Trending
GoodRx
GoodRx
GoodRx
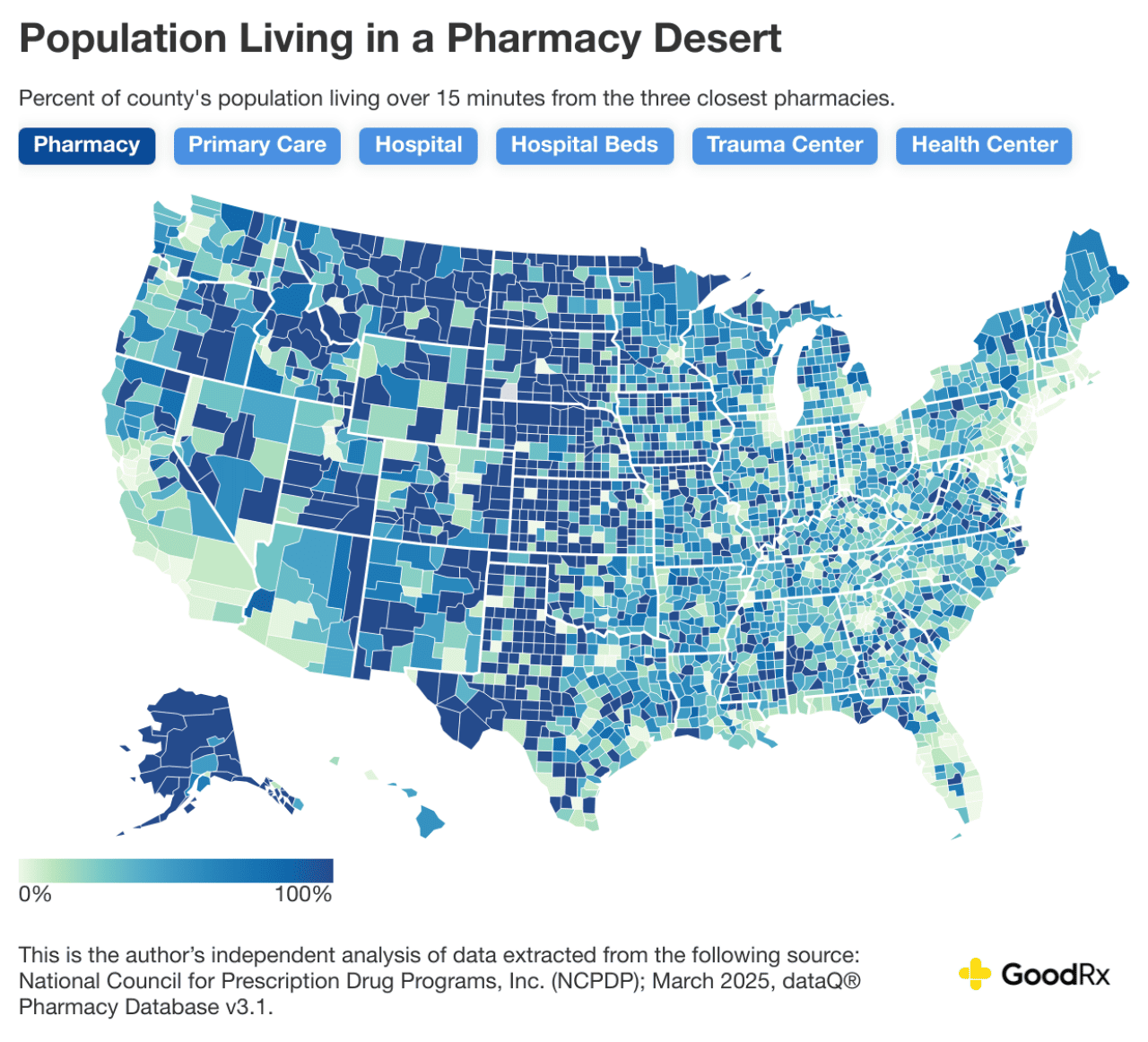
Pharmacy deserts
Since 2021, the large number of pharmacy closures throughout the U.S. has added a significant burden to healthcare access. Today, over 48 million people live in a pharmacy desert — up from 41 million in 2021. In the U.S., 45% of counties are pharmacy deserts, where the majority of residents have to drive over 15 minutes to reach nearby pharmacies — a distance that can make it difficult to fill a prescription, especially for those without reliable transport.
Similar to how people living in food deserts face barriers to following a nutritious diet, the farther a person lives from pharmacies, the less access they have to in-stock medications and different options for price shopping. This is especially concerning as medication shortages continue to impact Americans. A GoodRx Research survey conducted from February to May this year found that nearly 1 in 5 Americans had to visit multiple pharmacies in order to fill their prescription.
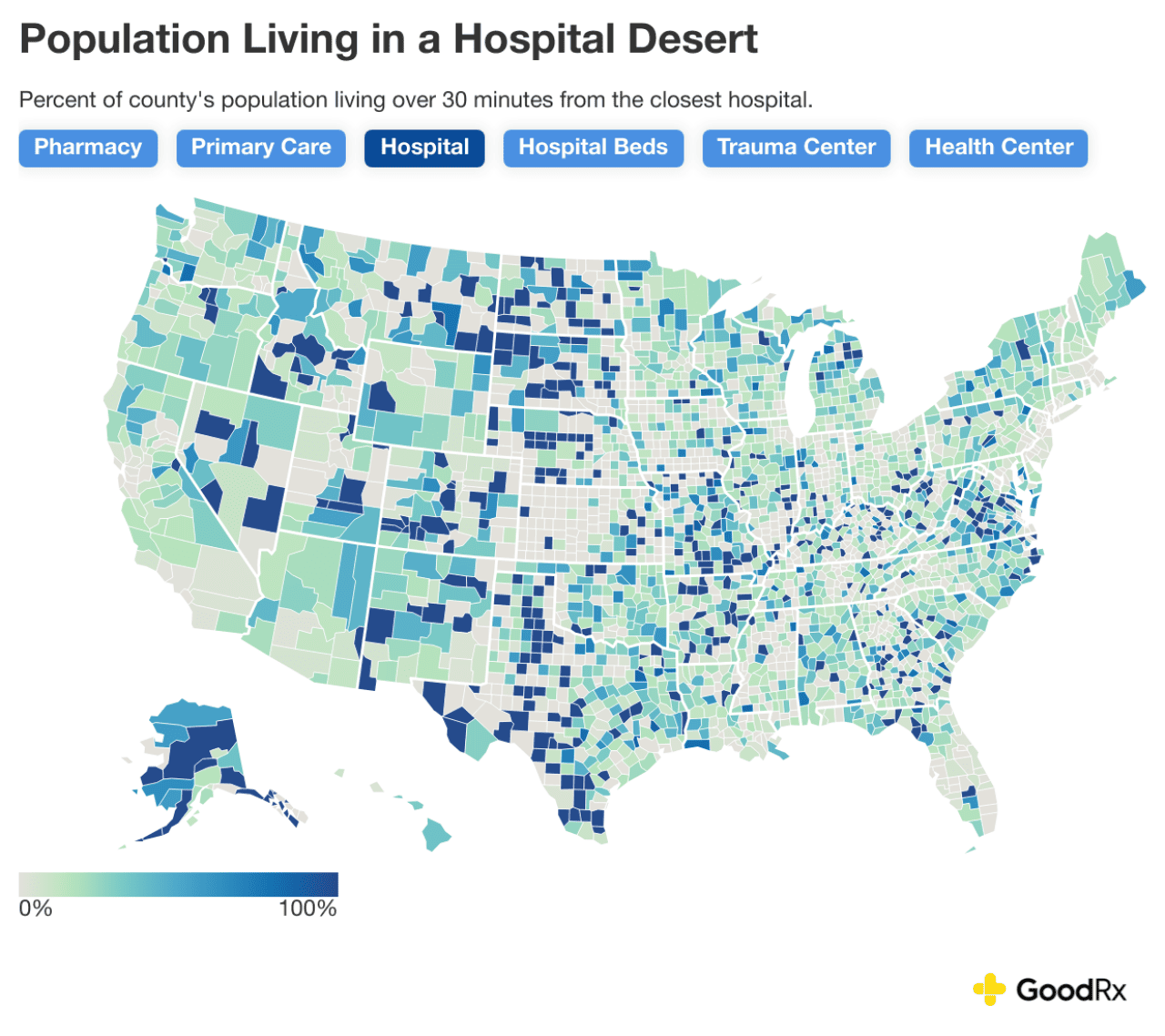
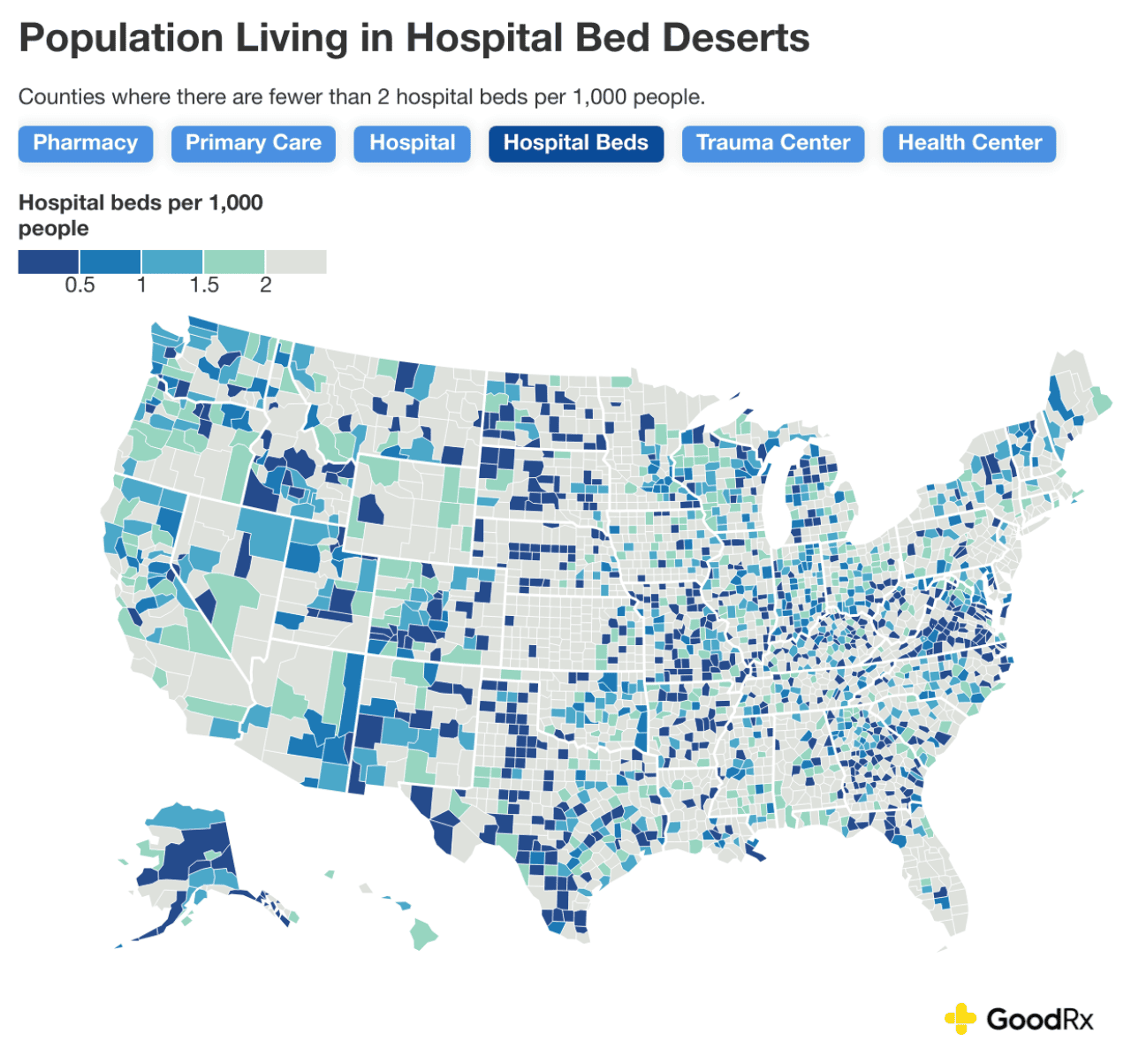
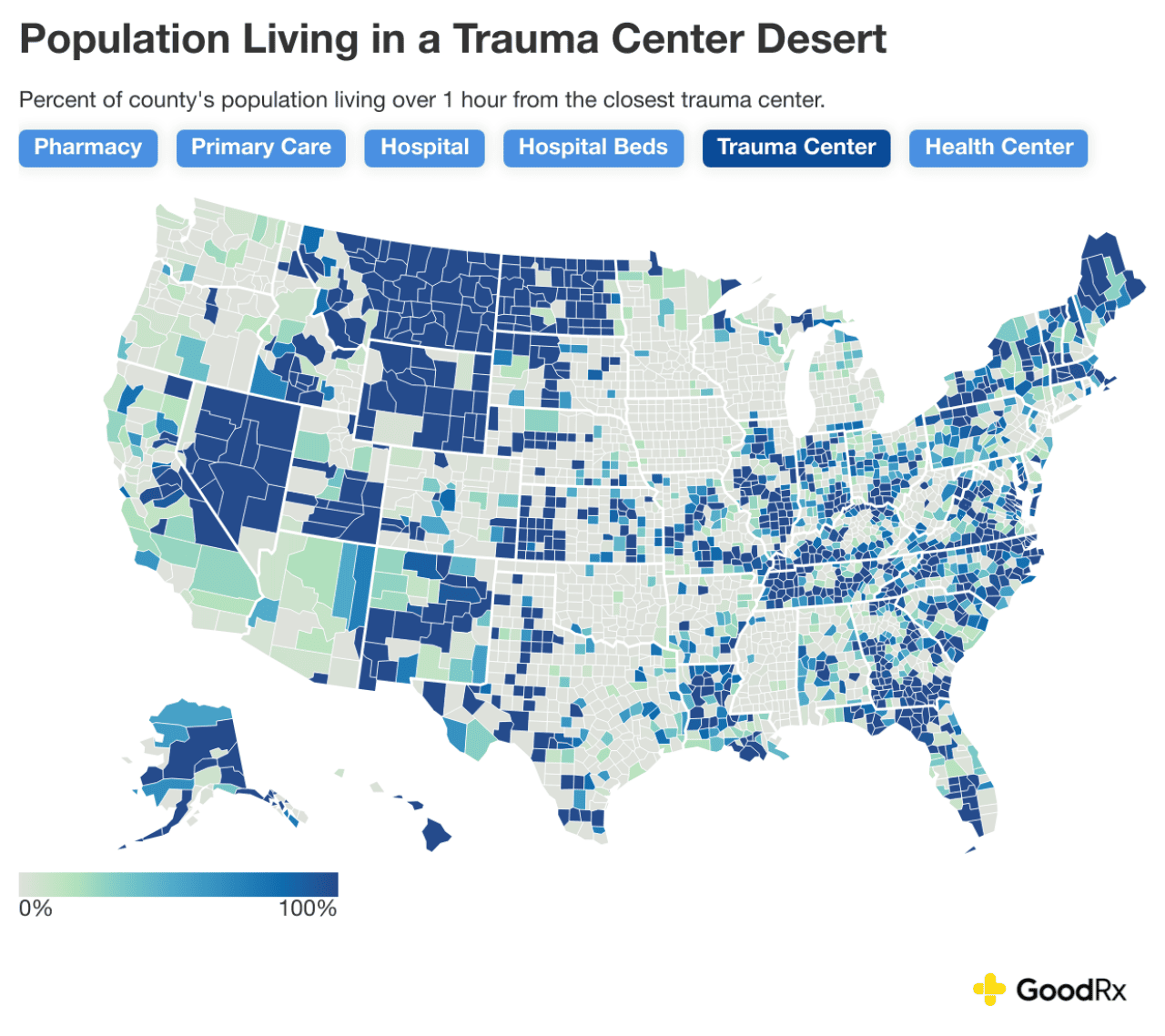
Hospital, hospital-bed, and trauma-center deserts
Access to hospitals and trauma care also has not improved since 2021. The number of people living in hospital deserts, hospital-bed deserts, and trauma-center deserts has remained roughly the same:
- Over 28 million live over 30 minutes from the nearest hospital.
- Over 79 million live in an area with fewer than 2 hospital beds per 1,000 people.
- Nearly 50 million live over one hour from a hospital equipped to handle major traumatic injuries.
Similarly, 20% of counties are still hospital deserts, 48% of counties are still hospital bed deserts, and 38% of counties are still trauma-center deserts for the majority of residents.
For these Americans, appropriate hospital care may be too far away to survive a serious injury or illness. Research shows that long travel times to the hospital negatively affect treatment and quality of care. And, when accessing a trauma center, every second counts. Doctors often refer to the “golden hour,” which is the concept that a patient needs to receive definitive care within an hour of injury to increase their chances of survival.
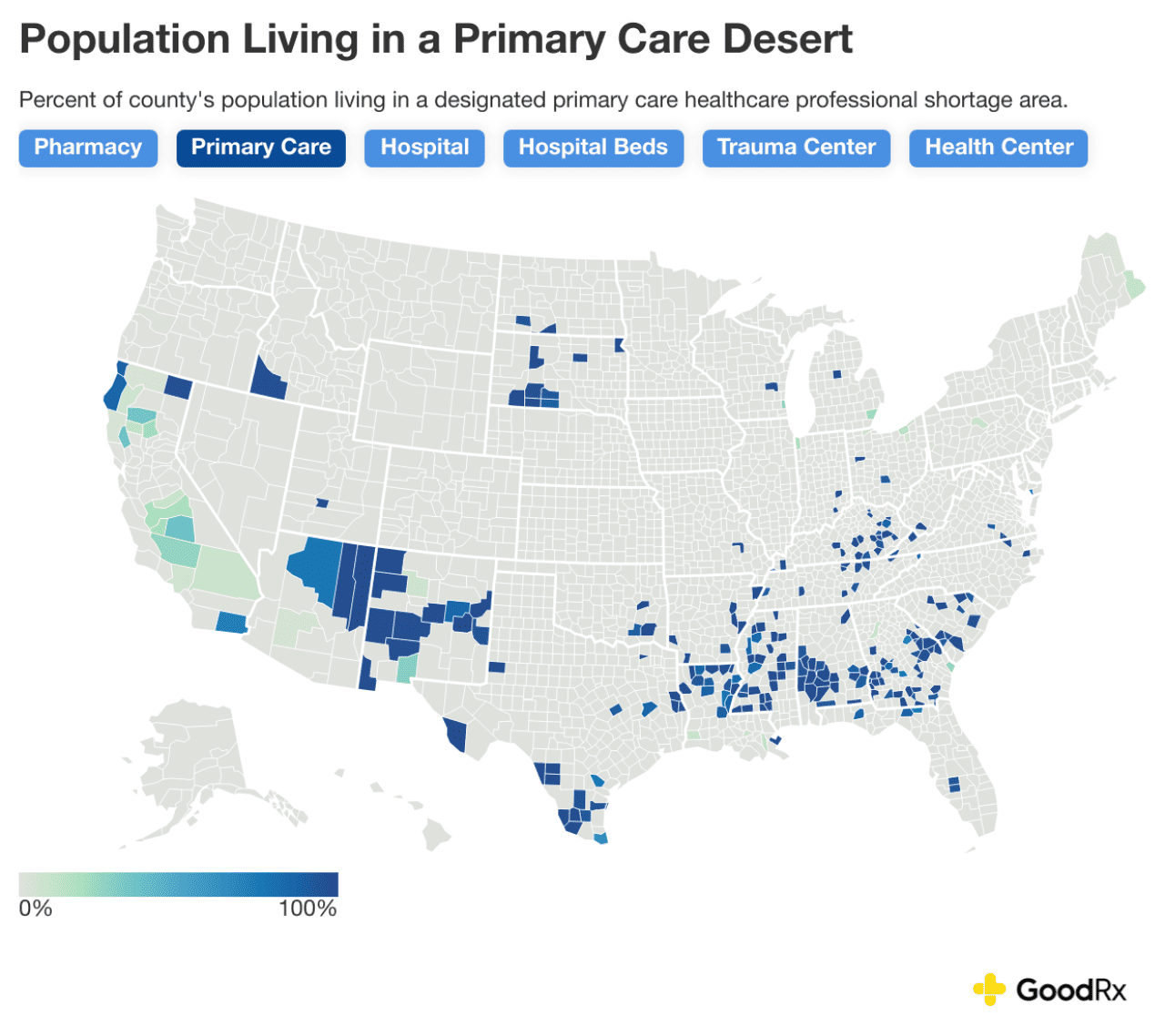
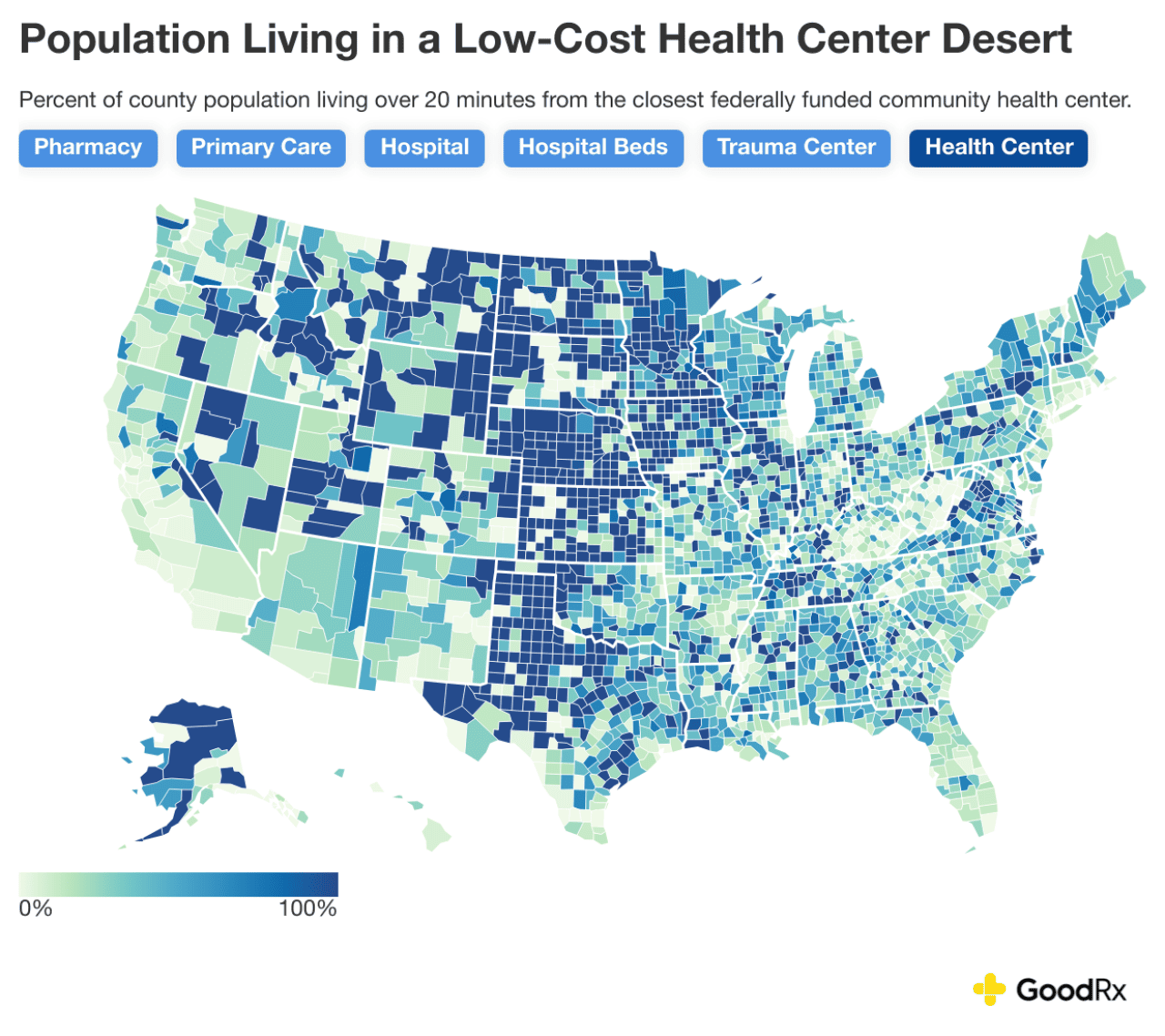
Primary care and community health center deserts
The number of federally designated primary care healthcare professional shortage areas has declined since 2021. However, this is largely due to a system reclassification that withdrew shortage designations in 2024 for many facilities — not because primary care shortages actually improved. In fact, according to the American Hospital Association, the number of staffed beds in U.S. hospitals has declined from 2021 to 2025. And, the average patient caseload in remaining federally designated primary care deserts — home to nearly 8 million people — is still one full-time primary care professional for every 7,597 people. That’s over 2.5 times the recommended level.
Meanwhile, federally funded community health centers have become slightly more accessible since 2021 — at least for now. While over 71 million people still live in health center deserts today, this number is down from over 78 million people in 2021. However, funding for these health centers and programs that address primary care shortages are currently at risk due to federal policy changes.
States hit hardest by healthcare deserts
Healthcare deserts across multiple services make it even harder for people to access comprehensive care. Almost 60% of counties have more than one type of healthcare desert, meaning people lack adequate access to more than one critical healthcare service. And nearly 8 million people live in counties with at least four healthcare deserts.
These states have an especially high share of the population living in some kind of healthcare-desert county:
- Wyoming: 87%
- Vermont: 74%
- Montana: 70%
- New Mexico: 60%
- Alaska: 56%
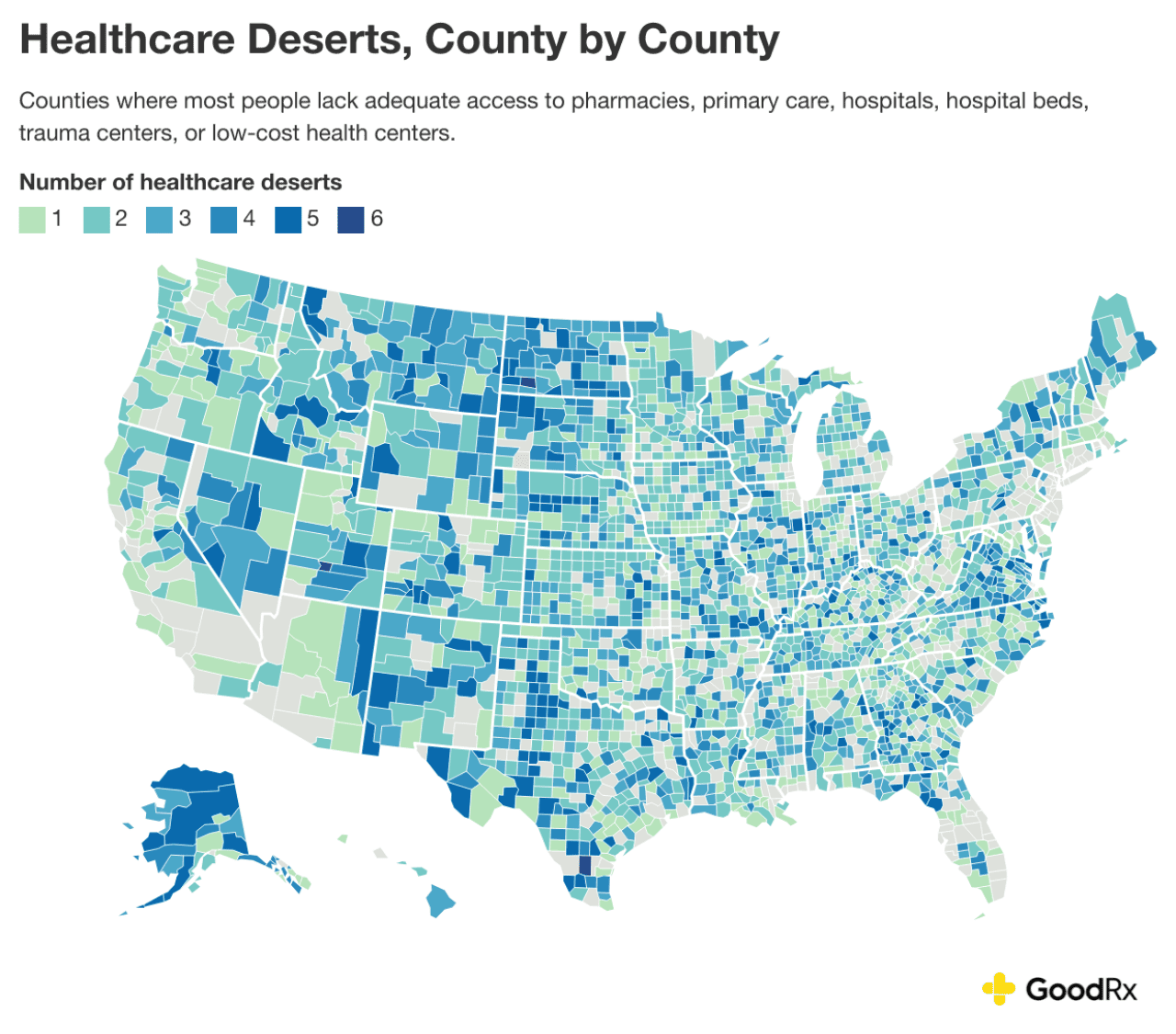
GoodRx
Specific counties across the U.S. also face widespread healthcare deserts. In New Mexico’s Catron County, over 3,500 residents face healthcare deserts in all services, from getting their prescription from the pharmacy to accessing primary and emergency care. It’s the same for the 11,000 residents of Duval County, Texas, and nearly 2,500 residents of Hettinger County, North Dakota. In these regions, accessing any kind of healthcare comes at an increased time and cost.
Who is most affected by healthcare deserts?
Healthcare access goes beyond having the requisite physical infrastructure. People may have difficulty actually using existing healthcare infrastructure because of personal or financial barriers. As a result, health disparities may persist even in places that aren’t considered “healthcare deserts,” simply because some groups still struggle to access the resources that are available.
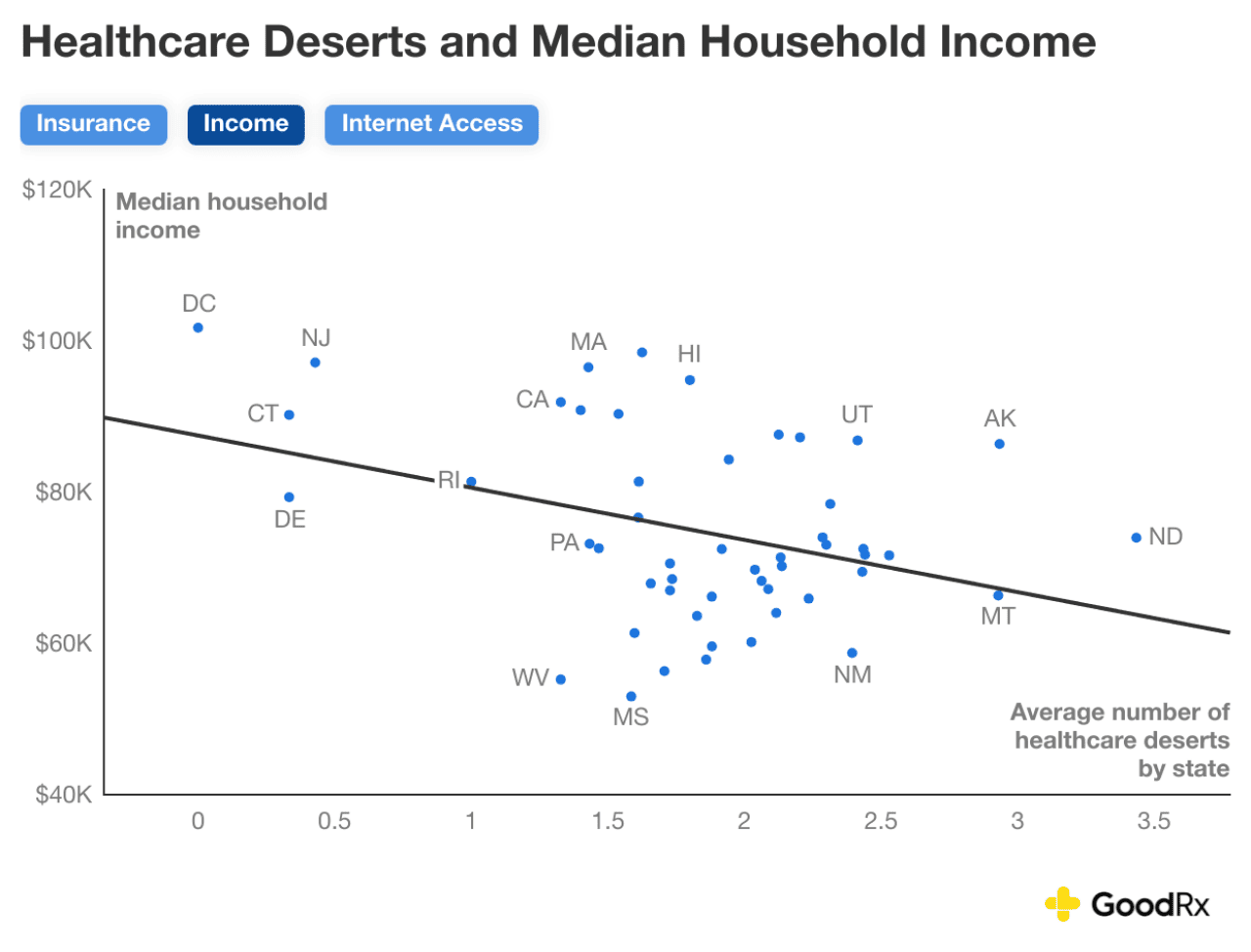
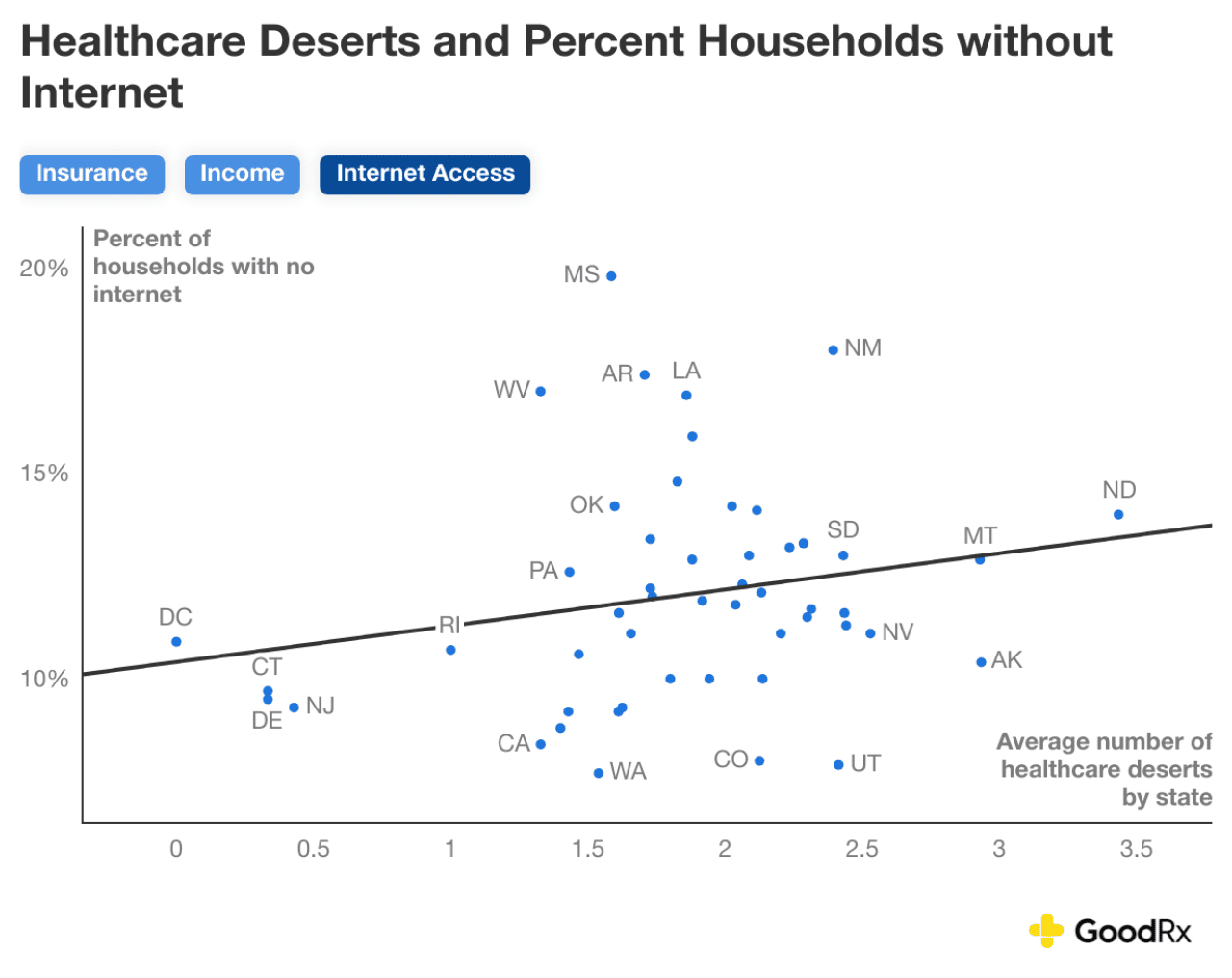
The charts below show the three factors that are more common in states with a higher number of healthcare deserts:
- Lack of health insurance
- Low household income
- Poor internet access
In all of these cases, residents in states with more barriers and more healthcare deserts will have an even harder time accessing the care they need.
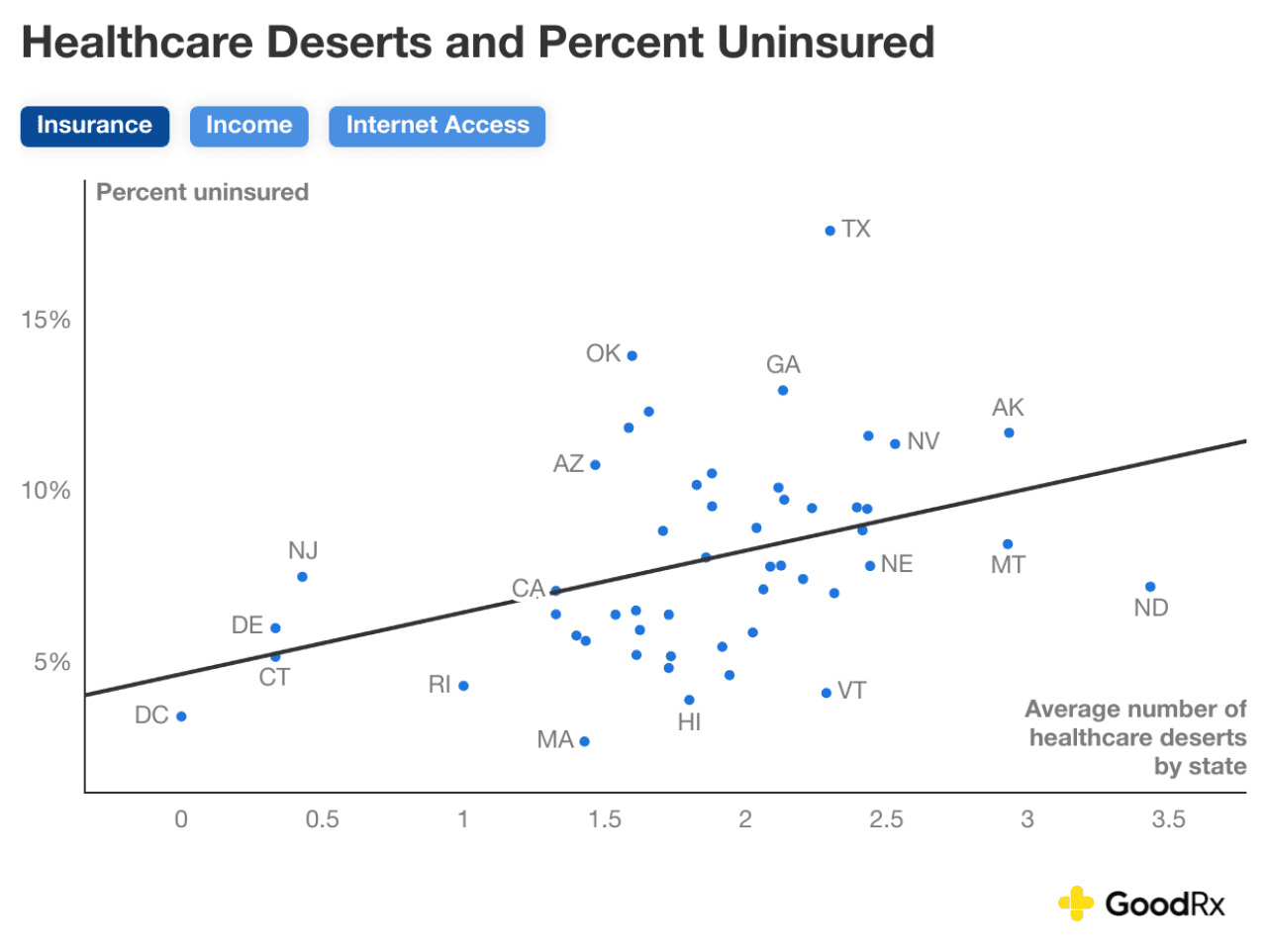
GoodRx
GoodRx
GoodRx
These trends have persisted since 2021. States with more healthcare deserts also tend to have larger uninsured populations, lower household incomes, and less broadband internet access. These financial obstacles, coupled with inadequate healthcare infrastructure, can make it even more difficult for people to get the healthcare they need.
The bottom line
Providing adequate care for individual and community health is an ongoing and multifaceted endeavor that implicates an array of healthcare services and providers. Healthcare deserts throughout the U.S. continue to pose serious challenges to this goal for millions of Americans.
The prevalence of healthcare deserts means that few actually have adequate access to all aspects of healthcare. So, while someone may live close to a pharmacy, they may have to drive over an hour to a trauma center if they get in a serious accident. Or if their doctor is just down the street, finding a pharmacy that stocks their prescription may require a longer drive. Lacking just one dimension of healthcare can be detrimental to the health of individuals and communities at large.
Co-contributors: Lauren Chase, Trinidad Cisneros
Methodology
Data on community retail pharmacies were sourced from DataQ and the GoodRx database. Data on primary care providers were sourced from Health Resources & Services Administration primary care health professional shortage areas. Data on hospitals and trauma centers were sourced from Homeland Infrastructure Foundation-Level Data and the Indian Health Service. Data on federally funded community health centers were sourced from HRSA and IHS. Demographic data on county population, internet access, household income, and insurance coverage were sourced from the 2020 and 2022 American Community Survey 5-year data.
Driving time to the nearest pharmacy, hospital, trauma center, and community health center was calculated based on the straight-line distance from each census tract population centroid. A detour index of 1.417 was applied to each driving distance. Driving time was estimated using average driving speed in urban, suburban, and rural areas. For driving time to trauma centers, ambulance driving speed was used.
Pharmacy, hospital, and trauma center deserts are geographical deserts based on driving time thresholds from each census tract population centroid. At the county level, a county is considered a healthcare desert if more than 50% of the county’s population lives in healthcare desert census tracts. The number of healthcare desert categories where the majority of the county’s residents live in a desert was used to count the total number of deserts per county.
For pharmacy deserts, a census tract is considered a desert if the average driving time to the three closest pharmacies exceeds 15 minutes. The average distance to the three closest pharmacies was used in order to account for pharmacies’ inventory, insurance preferred networks, and patients’ ability to price shop. The threshold of 15 minutes was based on the concept of “food deserts,” defined by the USDA as at least 500 people and/or 33% of a tract population residing more than 1 mile from a supermarket or large grocery in urban areas and more than 10 miles in rural areas. Fifteen minutes was derived by applying the average driving speed in rural areas to 10 miles.
For hospital, low-cost health center, and trauma center deserts, a census tract is considered a desert if the driving time exceeds 30, 20, or 60 minutes to the nearest hospital, health center, and trauma center, respectively. Based on previous studies, driving time exceeding 30 minutes to a hospital is considered a travel burden that can negatively affect timely diagnosis and quality of treatment (see Probst et al. (2007), Bosanac et al. (1976), and Ambroggi et al. (2015)). The driving threshold to community health centers was reduced in order to account for increased use by underserved and vulnerable populations, which have been shown to be more impacted by travel burden (see Martinez et al. (2003), Fitzpatrick et al. (2004), and Syed et al. (2014)). For trauma centers, a driving threshold was set at 60 minutes, as travel times over one hour have been associated with increased patient mortality among severely injured patients (see Sampalis et al. (1993), Crandall et al. (2013)).
For hospital bed deserts, a county is considered a desert if there are fewer than 2 beds per 1,000 population. According to 2020 data, the median number of hospital beds per 1,000 population among Organisation for Economic Cooperation and Development countries is 3.5. As the U.S. ranks in the bottom quartile with 2.8 beds per 1,000 people, a conservative desert threshold of fewer than 2 beds per 1,000 population was chosen. Note that this hospital bed threshold is also below World Health Organization recommendations. Hospital beds from all U.S. hospitals are included, including general acute care, long-term care, critical access, and psychiatric hospitals.
For primary care provider deserts, a county is considered a desert if more than 50% of the population lives in primary care geographic HPSAs. These areas are scored based on having a low population-to-provider ratio, high population share with income below 100% of the federal poverty level, high rates of infant mortality or low birthweight, and long travel times to the nearest source of care outside of the area.
This story was produced by GoodRx and reviewed and distributed by Stacker.
![]()






